
Testing whether "Tongkat Ali" actually is Tongkat Ali
A dubious study about Tongkat Ali and liver injury
Articles, videos about Tongkat Ali, Black Ginger, and Butea Superba
Articles, videos about optimal sex
Tuberculosis Treatment
Tuberculosis is a well-researched disease. You can read about it on many mainstream health websites.
The Mycobacterium tuberculosis by itself is not a controversial topic.
But treatment is. What public health institutions, from the WHO down to village healthcare workers, disseminate about
the treatment of tuberculosis is propaganda.
Propaganda is distorted information. The goal may be honorable: a worldwide decline of tuberculosis. But pamphlets aiming to promote
adherence to treatment regimens with statements like "Tuberculosis, otherwise deadly, can be cured with antibiotics" omit salient
points of what this "cure" means for many individual patients: the bacillus may be suppressed, at least temporarily, but their
overall health will be worse after chemotherapy than it was before untreated tuberculosis.
Physicians are complacent. Physicians have treatment guidelines, and these call for an aggressive drug treatment of tuberculosis.
Physicians will not risk their jobs or licenses by advising patients, that tuberculosis chemotherapy may do them serious harm.
Immediate chemotherapy may be best for the community and the goal of tuberculosis eradication, but all too often, it makes the patient
a sacrificed pawn.
If one wants to know what really is in store for those who agree to tuberculosis chemotherapy, one has to read the scientific literature. Articles
in scientific journals are usually not tuberculosis eradication propaganda, but intended for the scientific community, and to let physicians
know what the real score is.
The toxicity of tuberculosis drugs
"Most current TB regimens consist of six to nine months of daily doses of four drugs that are highly toxic to patients."
"Prolonged treatments with severe side effects reduce patients' physical and mental endurance during the course of treatment."
The four first-line drugs in tuberculosis chemotherapy are: Rifampin (Rifampicin), Isoniazid, Pyrazinamide, and Ethambutol.
Here first some rather harmless patient reviews.
For Rifampin:
For Isoniazid:
Scientific research into side effects is more scary.
Unfortunately, serious visual impairment, even blindness, is a potential side effect primarily of ethambutol, but
also of isoniazid
The common dosage for ethambutol is 15mg/kg bodyweight. Blindness can occur
even at that dosage. At dosages of 100mg/kg bodyweight, blindness is almost a certainty.
"We describe a 43-year-old man who developed signs and symptoms of bilateral optic neuropathy during treatment with ethambutol.
Ethambutol was initiated at a dosage of 15 mg/kg per day. Three months later, the patient had lower extremity neuropathy,
and 2 weeks after that he developed a rapidly progressive, severe decrease in vision... Visual acuity testing before initiation of treatment showed
20/20 vision in both eyes and normal color vision. Ophthalmologic examination [after ethambutol treatment] revealed a best corrected visual
acuity of 20/200 with the right eye and counting fingers at 4 feet [1.2 meters] with the left eye... Manifestations of toxicity can
occur as late as 12 months after initiation of therapy."
Here is what the American Academy of Ophthalmology has to say about ethambutol and blindness:
"The prevalence of EON [ethambutol-induced optic neuropathy, damage to the otic nerve] in patients treated for tuberculosis is
estimated to be 1-2%. According to the World Health Organization (WHO), there are around 9.2 million new cases of tuberculosis each year,
55% of which will take ethambutol. Given that the incidence of EON is about 1-2% among treated patients, these statistics suggest there could be as many as
100,000 new cases of EON annually. Furthermore, the risk of EON is highly dose dependent. The estimated prevalence of EON for ethambutol
doses of 15, 20, 25, and > 35 mg/kg per day are < 1%, 3%, 5-6%, and 18-33%, respectively. At any of the therapeutic antimicrobial dosing regimens,
there is a variable and sometimes idiosyncratic [unique to the individual patient] risk for EON and thus there is effectively
no truly “safe” dose for EMB. Other than ethambutol dosage, risk factors for EON include age greater than 65 years and hypertension... The visual acuity loss may vary from
minimal (20/25) to severe (no light perception) and the severity of the visual loss at onset is often mild and insidious... Finally,
multiple case reports have identified isoniazid, another first-line treatment for tuberculosis, as a cause of optic neuropathy
similar to EON. Therefore, patients taking ethambutol in combination with isoniazid may be at increased risk for visual loss."
Second-line aminoglycoside tuberculosis drugs are toxic to human hearing.
"Sixty four patients were put on second line aminoglycoside anti-TB drugs. These were divided into three groups: group I, 34 patients using
amikacin, group II, 26 patients using kanamycin and group III, 4 patients using capreomycin. Of these, 18.75% of the patients developed
sensorineural hearing loss involving higher frequencies while 6.25% had involvement of speech frequencies also.
All patients were seen again approximately one year after aminoglycoside discontinuation and all
hearing losses were permanent with no threshold improvement."
"A total of 42 Patients undergoing multidrug resistant tuberculosis treatment participated in the study... The study found 45.23% participants with some
degree of hearing loss consequent to multidrug resistant tuberculosis treatment. Around 9.5% of the total participants developed potential
disabling hearing loss."
The combined chemotherapy is toxic to the kidneys.
"The standard anti-tuberculosis (TB) regimen occasionally causes acute kidney injury (AKI). The major etiology is rifampicin-induced
acute interstitial nephritis... Among 1,430 patients with active TB, 15 (1.01%) developed AKI...
The renal function was normalized in 12 patients (80.0%) after restarting anti-TB treatment without rifampicin (n=12) or isoniazid (n=1).
Two patients died due to severe renal failure after restarting rifampicin."
A drug (toxin) that comes with a definite risk of acute kidney injury is likely to be detrimental to kidney function even when acute kidney
injury does not occur.
"TB patients had a significantly higher risk of developing CKD [Chronic Kidney Disease] than the general population."
Standard tuberculosis therapy is also toxic to the liver.
"Drug-induced liver injury (DILI) is a common complication of tuberculosis treatment... A total of 58 of 1928 (3.0%) patients met the criteria for
DILI defined in this analysis."
There are hundreds of potential side effects for the combined tuberculosis drugs. Acute kidney injury may only occur in 1 percent,
tragic enough. But the risks add up, with possible permanent blindness and deafness standing out, and it is very unlikely indeed,
especially for older patients, that they get through tuberculosis chemotherapy unscathed.
"Side-effects such as hepatitis [liver inflammation], dyspepsia [stomach pain that often gets worse with eating], exanthema [widespread skin rash]
and arthralgia [joint pain] were responsible for termination of therapy in up to 23% of patients during the intensive phase... The side-effects
profile of TB chemotherapy is magnified in... those being treated with second-line drugs for multidrug-resistant TB, during which as
many as 86% of patients may develop medication side-effects."
Because of the severe side effects of tuberculosis drugs, it is not surprising that many people just don't want to take them... and then omit dosages,
or the whole drug regimen.
The WHO, determined to reduce tuberculosis counts, thus devised a protocol for dealing with such recalcitrants:
DOT - directly observed therapy, or DOTS - directly observed therapy short course (an euphemism, to put it mildly, as
this "short course" typically means 6 months of chemotherapy).
"Observed therapy" means that patients are required to go to a healthcare facility and obtain their medication from a nurse who
makes sure that the pills are actually swallowed. And if the patient does not show up, then the nurse may look for them at home.
Kind of "enhanced persuasion" so that patients take their meds, in spite of the side effects.
There are ethical implications in such tactics.
"Research from Ethiopia and Norway demonstrates that the rigid enforcement of directly observed treatment conflicts with patient
autonomy, dignity and integrity... Many [patients] reported being threatened, punished, humiliated or treated angrily by staff for not adhering
strictly to the implicit rules of the system... As in Ethiopia and Norway, there are still many examples of health personnel responding to
such needs [of personal adjustments] by the use of threats, scolding and increased rigidity..."
Problematic antibiotics
For many therapies, newer drugs are superior to older drugs (eg benzodiazepines versus barbiturates), with a safer
side effects profile.
That paradigm doesn't apply to antibiotics used to treat tuberculosis. The side effects of second-line or third-line medications
for tuberculosis are just as miserable, or even worse, than those considered first-line treatments.
"The therapeutic approach for drug-resistant tuberculosis is cumbersome, because of the poor, expensive, less-effective,
and toxic alternatives to the first-line drugs."
The original location of the clip is: https://youtu.be/3-KsGYRgSno
Médecins Sans Frontières (Doctors Without Borders in English) is an international charity for medical care.
For their activities, including tuberculosis treatment, they seek donations.
"Private donors provide about 90% of the organisation's funding, while corporate donations provide the rest, giving MSF an annual budget
of approximately US$1.63 billion.
The charity is doing many good things with all of this money.
However, the two medications they refer to in the above video clip, bedaquiline and delamanid, are no wonder drugs.
And anyway, they have to be combined with first-line drugs (called background treatment), including the one that carries the highest risk
of vision loss (ethambutol).
While in combination with first-line drugs, they often are effective against multidrug-resistant tuberculosis, they also come with their
own dangerous side effects, such as potentially fatal heart arrhythmias.
"Drug interactions with other hepatotoxic agents like pyrizinamide and drugs that prolong QT interval like fluoroquinolones,
clofazimine can potentially be catastrophic in MDR-TB patients [multi-drug resistant tuberculosis]."
To avoid the side effects of drugs that don't help, it would be nice if it could be tested whether the bacterial strain by which a patient
is afflicted is susceptible or resistant to a certain drug. Unfortunately, medical science at the current state of the art is
not sophisticated enough for that.
"... the reliability of DST [drug susceptibility testing] results obtained through widely used methods does not meet acceptable levels,
except for DST to isoniazid and rifampicin... Poor reliability stems from a weak correlation with clinical response and a low
reproducibility due to the poor standardization of the complex and fragile test procedures... Most of the currently used DST methods
suffer from low predictability associated with clinical irrelevance of the results..."
Thus, in clinical practice, physicians just prescribe what, in their experience, usually works, and hope for the best.
And if, after a few months, they find out that, in spite of all the side effects, the bacterial load does not drop, they initiate
a next round of drugs, and if that also doesn't do it, they switch to the third set. They will continue like that until a
patient succumbs to any of his or her morbidities, tuberculosis by then just being one of many.
The drugs anyway do NOT cure tuberculosis
The illusion created by public health institutions and physicians goes like this:
You take your pills for 6, 9, or 24 months, and after that, you are cured of tuberculosis.
But fact is, you aren't. A negative smear test doesn't mean a person is free of bacilli in the lungs. If there are fewer than 5000 bacilli
per mL specimen, a test for acid-fast bacteria will likely be negative.
"Smear microscopy... requires 5000–10,000 bacilli per mL of sputum for showing a positive result."
But in "healed", just as in latent infections, bacteria lie dormant at locations where their presence
cannot be tested. They can also not be killed by chemotherapy that targets metabolic processes of Mycobacterium tuberculosis, simply
because dormant bacteria have no metabolism worth mentioning. Such bacteria are called persisters.
There is a definite chance that, at a time the host immune system is weakened, the disease will come back in its active form.
"The recurrence incidence was 8.3% and in 85.9% of these patients, it occurred in the time interval of 1-5 years after successful treatment."
A 2012 study on persisters prominently quoted Walsh McDermott: "When one realizes that, even though the bacilli vanish and
there is … truly latent infection, the bacilli are, nevertheless, still there … drug susceptible, I think you will agree with me that
it shows that ‘you can't win.’"
"The outcome of M. tuberculosis infection is often a state of equilibrium characterized by immunological control and bacterial persistence."
That is the best one can get: a stalemate. And that is the same for drug-treated tuberculosis and self-healed tuberculosis
(with supportive measures, such as bed rest).
Another pharmaceutical strategy
There is something intrinsically problematic with the antibiotics used for toxic tuberculosis chemotherapy, and it's
not that these antibiotics per se would be so much worse than other antibiotics.
It's rather that the tuberculosis bacillus doesn't lend itself easily to the whole concept of antibiotic treatment.
Normal bacteria, even if they kill a human host only after decades, like Treponema pallidum which causes syphilis, exist in the
human host in a uniform metabolic state. And if the strain is not resistant, as soon as a suitable antibiotic is applied, most of the
bacteria are dead in a few days, and all are eliminated in one to two weeks.
Mycobacterium tuberculosis is not like that. It exists in the host in different metabolic states, from actively
dividing in a day or so, to lying dormant for years with practically no metabolism, and possibly a variety of transition phases.
As antibiotics typically target metabolic processes, dormant bacteria, which don't have any, are out of reach for the drugs.
But in an immune system already thrown off balance by medications, some bacilli, here and there, awake from their dormancy,
and start replicating.
Thus, the WHO decides that a full cocktail of antibiotics should be taken from 6 months (they call this "short course")
to 2 years, or even longer.
Now, at such a long regimen, serious side effects will appear with any antibiotic, not just those used for tuberculosis.
So, maybe something is wrong with the antibiotics approach, which actually competes with the host immune system on how to handle the pathogen.
Maybe it would make more sense if physicians were to support the host's biology in a manner that suppresses
Mycobacterium tuberculosis, rather than compete for the trophy of victory.
Such an approach already has a name: host-directed therapies
But most certainly, they aren't mainstream.
The famous scientific journal Nature, in a 2017 article, on host-directed therapies in the context of tuberculosis:
"Host-directed therapy (HDT) is an emerging approach in the field of anti-infectives. The strategy behind HDT is to interfere with
host cell factors that are required by a pathogen for replication or persistence, to enhance protective immune responses against a pathogen,
to reduce exacerbated inflammation and to balance immune reactivity at sites of pathology... To overcome Mtb resistance to killing
by macrophages and to promote Mtb entry into autophagic compartments, a diverse range of pro-autophagic drugs has been proposed
for TB management by HDT... Currently, the most promising drug that induces autophagy and promotes phagosome maturation of Mtb-infected cells is the
oral biguanide metformin, which is widely used for the treatment of type 2 diabetes. Metformin activates
5'-adenosine monophosphate-activated protein kinase (AMPK) and interferes with the mitochondrial respiratory chain, promoting the
production of reactive oxygen species (ROS) and subsequent Mtb killing in human and murine macrophages. To a certain extent,
metformin restricts bacillary growth in murine pulmonary TB. Given its widespread application and acceptable safety profile,
metformin seems to be ready to enter clinical trials as an HDT for TB."
Yes, Mycobacterium tuberculosis, by secreting specific molecules, blocks autophagy (the destruction of unwanted
intracellular material, including pathogens). Interestingly enough, the anti-tuberculosis effects of curcumin
(the active compound in turmeric) have been linked to its capability to induce autophagy in tuberculosis-infested calls.
"We found that curcumin enhanced the clearance of MTB [Mycobacterium tuberculosis] in differentiated THP-1 human monocytes and
in primary human alveolar macrophages. We also found that curcumin was an inducer of caspase-3-dependent apoptosis and autophagy.
Curcumin mediated these anti-MTB cellular functions, in part, via inhibition of nuclear factor-kappa B activation."
More on turmeric later in this review.
"Untreated" tuberculosis
"Untreated" in this context refers only to tuberculosis not treated by chemotherapy.
In light of the severe and potentially life-shortening side effects of tuberculosis chemotherapy, the prognosis of
untreated tuberculosis is important to know.
There are no studies on the mortality of untreated tuberculosis conducted in the past 80 years, since chemotherapy has become
available. All studies on untreated tuberculosis were done in the first half of the 20th century. These studies, however, have been
extensively analysed in the past few years.
A 2011 review:
"Taking the crude unweighted average of all studies one arrives at a 5-year case fatality of 58% and a 10-year case fatality of 73%
for open (smear-positive) tuberculosis. Taking an average weighted by sample size these numbers are 55% and 72% respectively.
Of course, these mortality data are somewhat distorted by mortality from other causes,
as most studies do not record cause of death, and all-cause mortality rates may have been somewhat higher in
the pre-antibiotic era than they are now... On the basis of the above data, especially the studies by Berg, Thompson, and Buhl
and Nyboe which – unlike studies on sanatorium patients – appear to be mostly population based, a 30% 10-year survival for
smear-positive patients, i.e. a 70% CF [case fatality], as used by WHO and others in their estimates of the burden of tuberculosis,
seems a reasonable ballpark figure. As tuberculosis is mostly a disease of young to middle-aged adults the distortion by other causes of death
is probably small."
A 2023 analysis:
"Pre-chemotherapy era data are a rich resource on survival of people with untreated TB... We found 12 studies with TB-specific mortality data.
Ten-year survival was 69% in North America and 36% in Europe... Geographically, people in North American studies experienced better
outcomes than those in Europe. This may be because North America was more shielded from the worst effects of the two world wars in
the early twentieth century than Europe."
The same study, however, found a marked difference in the 10-year survival rates of "untreated" patients in sanatoria, compared to those
who remained untreated at home.
"Only 38% of non-sanitorium individuals survived to 10 years compared to 69% of sanitoria/hospitalized patients..."
Bed rest (see below) likely accounted for the way-better survival chances of patients in sanatoria or hospitals.
To compare untreated and treated tuberculosis, the 10-year survival rates after "successful chemotherapy" are of interest.
"The median of survival time after successful treatment was 10.5 years and survival probability for 11 years after successful treatment was 70%...
This study showed that positive smear pulmonary tuberculosis even after successful treatment has an adverse effect on the patients’
survival and leads to a decrease in their survival rate in the long run."
"We used local health authority records from 3 US sites to identify 3853 persons who completed adequate treatment of TB and
7282 individuals diagnosed with latent TB infection 1993 to 2002... We found more all-cause deaths (20.7% vs 3.1%) among posttreatment
TB patients than among the comparison group... Fully treated TB is still associated with substantial mortality risk.
Cure as currently understood may be insufficient protection against TB-associated mortality in the years after treatment."
"Based on a retrospective cohort study, information of 2,299 TB patients that had been referred to and treated at the NRITLD
[National Research Institute of Tuberculosis and Lung Disease], Masih Daneshvari Hospital [Teheran, Iran], from 2005 to 2015, was collected...
This study was done on 2,299 patients with treated pulmonary TB; 770 patients (33.49%) expired and 134 patients (5.83%) had disease relapse."
In the Iranian study, the ten-year survival rate of tuberculosis patients undergoing chemotherapy was 66.51%. That is even worse
than the ten-year survival rate of 69% in North American sanatoria in the pre-chemotherapy era.
Subclinical tuberculosis
An article in the scientific journal The Lancet Respiratory Medicine estimated that every year, about 12 percent of
patients with tuberculosis experience self-cure, without any toxic chemotherapy.
"Reversion from microbiologically positive to undetectable disease in prospective cohorts occurred at an annualised rate of 12% (6·8–18·0).."
When considering untreated tuberculosis, now or before, one aspect of relevance is and was the severity of the disease in
the individual patient.
Young and middle-aged adults may become violently ill, and the worse their condition, the worse the prognosis
when not treated by chemotherapy. On the other hand, the symptoms of active tuberculosis are often mild in
elderly populations (see below).
Tuberculosis with mild symptoms apparently is much more common than most people realize. Such cases are typically only found
after extensive x-ray screening of the population.
"Subclinical pulmonary tuberculosis, which presents without recognisable symptoms, is frequently detected in community screening...
Individual participant data were obtained and included for 12 surveys (620 682 participants) across eight countries in Africa and four in Asia.
Data on 602 863 participants were analysed, of whom 1944 had tuberculosis. The unadjusted proportion of subclinical tuberculosis
[mostly no persistent cough] was 59·1%... The majority of people in the community who have pulmonary tuberculosis do not report cough,
a quarter report no tuberculosis-suggestive symptoms at all..."
Here is how the numbers are to be understood: "602 863 participants were analysed, of whom 1944 had [active] tuberculosis". That is 1 in 310
screened patients, which translates as a tuberculosis prevalence of 322 in 100,000 people. These numbers are on top of those people
who seek medical treatment for tuberculosis on their own, not waiting for community screening.
The global average is 133 cases per 100,000 people.
Countries with the highest incident rates are The Philippines (638 cases per 100,000), North Korea (513), Gabon (509),
South Africa (468).
"An estimated 40% of people who developed TB in 2021 were not diagnosed or treated."
These 40% were discovered during routine population screenings. For many of them, their symptoms were not severe enough to seek help
at hospitals. It is not known how many of them were enrolled for chemotherapy in spite of non-severe symptoms.
The WHO estimates that in 2023, some 10.5 million people presented with new active tuberculosis,
and some 1.6 million died of the disease. This number likely includes people who died during tuberculosis treatment,
from either tuberculosis or the toxic side effects brought about by the treatment. It likely excludes people who died after
"successful" treatment for tuberculosis but suffered organ damage from a toxic drugs regimen that caused death after a few years.
Tuberculosis is a continuum
Public health officials, from the WHO down to village healthcare workers have a set of goals that they try to achieve
with their tuberculosis propaganda. They include:
* Get as much people as possible tested for tuberculosis, even those who have no clinical symptoms.
* Make people believe that tuberculosis is an infection that can easily be cured with antibiotics. The mantra is: take your pills,
and after 6, 9, or 24 months, you are healthy, and you can continue your life of before the tuberculosis diagnosis, just as if nothing has happened.
* Persuade people who are diagnosed with "active" tuberculosis, even if there are no symptoms or only minor symptoms,
to start full chemotherapy for 6 month.
* Convince people who have just "latent" tuberculosis, as does a quarter of all mankind, to nevertheless undergo tuberculosis chemotherapy.
Public health officials and complacent physicians usually omit warnings about the severe, toxic side effects from their
"information" or "consultation".
But tuberculosis is not a disease that you either have or don't have, just like gonorrhea or AIDS.
But even though it is caused by bacteria, tuberculosis presents more as a chronic condition, like type 2 diabetes, which is a
continuum that can range from a suboptimal insulin response to blood sugar values that cause blindness and death from kidney failure.
The gold standard of a tuberculosis diagnosis for the past 100 years or so has been the so-called smear test, in which sputum is
examined in acid-fast stain microscopy for Mycobacterium tuberculosis.
The specific sensitivity of the test requires at least 5000 bacilli per mL of sputum, otherwise if will produce a negative result.
Sure, with 30,000 or 40,000 bacilli per mL of the specimen, tuberculosis is easy to diagnose.
But whether a patient on a given day may have 4700 or 5600 bacilli in a sputum sample, and thus test positive or negative, is probably a
matter of luck.
Nevertheless, "sputum conversion" from a positive to a negative result after 2, 3, or 4 months typically determines
whether tuberculosis chemotherapy was "successful" or not.
But a tuberculosis relapse from below 5000 bacilli per mL of sputum to above 5000 is not an either/or difference, but just a gradual one.
Awareness is now growing that tuberculosis is not an either/or (you have it or you don't) disease.
It's not even an either/or/or disease (either no tuberculosis / or latent tuberculosis / or active tuberculosis) disease.
The whole thing is a continuum, ranging from no infection to dying from tuberculosis, and many nuances in between.
Here a scientific source for this view:
"Recent evidence indicates that the spectrum from TB infection to TB disease is much more complex, including a “continuum” of situations
didactically reported as uninfected individual, TB infection, incipient TB, subclinical TB without signs / symptoms, subclinical TB
with unrecognised signs / symptoms, and TB disease with signs / symptoms... These situations are regulated from one side by the
metabolic activity of Mtb (dormancy, intermittent replication, active replication) and from the other side by the host innate and
acquired immunity (which fights to limit the consequences of TB infection)... Subclinical TB had been described as a stage preceding
detectable active TB by a couple of weeks or months. This is probably inaccurate as some individuals with subclinical TB never
reach the status of TB disease “with symptoms” or spontaneously regress to latent TB (or even to the uninfected stage) without being ever
diagnosed with TB." Tuberculosis in elderly populations
Tuberculosis in the elderly population often presents with fewer symptoms.
"Symptoms of active TB are nonspecific and less pronounced in the elderly."
"Difficulties in diagnosis tuberculosis in older adults has been assessed in a meta-analysis of studies focusing on tuberculosis
in older adults, which found that common symptoms used to identify tuberculosis such as dyspnoea [shortness of breath], haemoptysis [coughing blood]
and fever are less prominent in older than in younger adults."
“Classical symptoms of TB (cough, haemoptysis [coughing blood], fever, nights sweats and weight loss) were less common among older patients with
pulmonary TB (PTB)... For those with PTB, chest radiography findings showed that cavitation and lymphadenopathy were more common among younger
patients. Conclusions: Older patients aged 65 years with TB had fewer “classical” clinical and radiological presentations of TB, which
may explain longer times to starting treatment from symptom onset compared with younger patients aged 65 years... TB in the elderly presents
with fewer of the classical symptoms of TB, less specific radiological changes... and it has even been proposed that TB in older adults
should be considered as a different disease entity."
By and large, elderly patients feel less discomfort with tuberculosis than are younger patients. This changes dramatically as
soon as standard chemotherapy is initiated.
"According to our findings, there is an increasing risk of TB-drug adverse events when age increases. In previous reports, the occurrence
of any major side effect has been associated with age, especially amongst the elderly. The frequency of adverse reactions has
shown to increase in a progressive and direct form in relationship to age."
It appears that in elderly patients, the definite discomfort of the tuberculosis disease really sets in as soon as the treatment starts.
But it is safe to assume that public health institutions and physicians are more concerned about containing TB in communities
than the comfort of patients. Public health institutions advocate aggressive pharmacological treatment of tuberculosis in elderly patients
not because it would add to the quality of life of elderly patients but because elderly patients on a highly toxic drug cocktail are less
contagious.
The other "tuberculosis"
Unfortunately, a substantial number of patients who are diagnosed with, and treated for, tuberculosis actually do not have the disease.
Because of their misdiagnoses, not only are they subjected to many medication side effects; those toxic medications also do not work properly because they are directed at the wrong pathogen.
This is a tragic constellation that may kill a patient faster than if he or she were left untreated.
Tuberculosis is caused by a pathogen called Mycobacterium tuberculosis. This bacterium belongs to a genus of more than 190 species.
Most of these bacteria are ubiquitous in nature and do not cause disease in humans. Only two species in the genus Mycobacteria are Obligate pathogens that need mammalian hosts, preferably humans, to complete their life cycles, Mycobacteria tuberculosis and Mycobacteria leprae.
Apart from that, there are other species of mycobacteria that are facultative pathogens. These do not need a host to complete their life cycles, but if a host is available, they adapt to the situation, and cause disease.
Tuberculosis can be diagnosed by clinical symptoms, which is very vague, or by microscopy, which, unfortunately, is also vague.
The most common non-tuberculous pathogenic mycobacteria are Mycobacteria avium species. They are grouped as Mycobacteria avium complex.
In microscopy, it is not possible to differentiate properly between Mycobacterium tuberculosis and Mycobacterium avium.
The most common microscopic diagnosis of tuberculosis relies on acid-fast staining by the Ziehl-Neelsen method. The same results show for all bacteria with cell walls of mycolytic acid.
Public health officials and physicians are over-proportionally interested in tuberculosis as this is a contagious disease, while a Mycobacterium avium complex infection is not.
Thus, there is a pronounced tendency in developing and even middle-income countries to consider all lung infections that show mycobacteria in smear or culture microscopy as tuberculosis, and treat the patient with the whole range of toxic anti-tuberculosis drugs, even if his or her lung condition is caused by Mycobacteria avium.
There is no data on how common Mycobacteria avium complex disease is in low and middle-income countries. Only one study concerned itself with the epidemiology of non-tuberculous mycobacteria (NTM) disease.
"The epidemiology of NTM disease has been difficult to determine because, unlike tuberculosis, NTM infections are not reportable in most states and countries. To obtain prevalence estimates, studies have used large [insurance] claims databases and NTM isolation rates from various geographic catchments. Most such studies have identified increases in the prevalence of NTM-PD [non-tuberculous pulmonary disease].
In the US and other countries with a low or moderate prevalence of tuberculosis, the incidence of NTM has risen dramatically since the 1990s. Data from Japan show a sharp increase in NTM-PD beginning in the mid-1990s, with a dramatic increase in incidence in 2014 that was 2.6 times that in 2007. The same study showed that, beginning in the 1990s, culture- and smear-positive cases of tuberculosis declined markedly. Similarly, the incidence of NTM-PD in Taiwan increased significantly, from 1.26 cases/100 000 patients in 2006 to 7.94 cases/100 000 patients in 2008.
Data from Ontario, Canada, show increases in both the annual isolation and prevalence of pulmonary NTM. The mean annual increase in isolation of pulmonary Mycobacterium species was 6.3% between 1998 and 2010, and the 5-year prevalence rate of NTM-PD rose significantly, from 29.3 cases/100 000 persons for 1998–2002 to 41.3/100 000 persons for 2006–2010. Data from the US show a similar trend in increasing NTM incidence...
The likely reasons for the increase in incidence of NTM are multifactorial: Better detection and recognition among clinicians and radiologists, changes in environmental NTM exposure, an aging population, higher incidence of underlying chronic lung disease, and more patients with suppressed immune systems are all contributory factors... NTM-PD primarily affects people ≥60 years of age..."
There are indications that throughout history until today (especially in low and middle income countries), many, often older, patients with non-tuberculous pulmonary disease were and are diagnosed with tuberculosis.
A previously quoted study concluded:
"Classical symptoms of TB (cough, haemoptysis [coughing blood], fever, nights sweats and weight loss) were less common among older patients with pulmonary TB (PTB)... Conclusions: Older patients aged 65 years with TB had fewer “classical” clinical and radiological presentations of TB, which may explain longer times to starting treatment from symptom onset compared with younger patients aged 65 years... TB in the elderly presents with fewer of the classical symptoms of TB, less specific radiological changes... and it has even been proposed that TB in older adults should be considered as a different disease entity."
This makes sense because indeed, the different disease entity, namely non-tuberculous pulmonary disease not only affects primarily older adults but often only presents with milder symptoms. For example, hemoptysis [the coughing of blood] is a hallmark of tuberculosis but is not common in patients with Mycobacterium avium.
"Although distinct, Mycobacterium tuberculosis and Mycobacterium avium both infect and survive in host macrophages. M. tuberculosis is more virulent, specifically adapted to humans, and grows poorly outside of the host. In contrast, M. avium can survive in the environment and also can infect several different host species in addition to humans, including birds, pigs, dogs, and monkeys."
The treatment of Mycobacteria avium complex pulmonary disease is similar to the treatment of tuberculosis, with one important difference: the main antibiotic is a macrolide, either clarithromycin or arithromycin.
"Treatment of MAC-PD typically comprises a macrolide, a rifamycin and ethambutol. In nodular-bronchiectatic MAC-PD, clinical guidelines give a conditional recommendation for these drugs to be taken three times weekly, whereas a daily regimen is recommended for advanced or severe nodular-bronchiectatic MAC-PD. In cavitary NTM-PD, intravenous amikacin or intramuscular/intravenous streptomycin may be given in addition."
The presumed necessity of the macrolide antibiotic suggest that standard tuberculosis treatment with the four first-line drugs isoniazid, rifampicin, ethambutol, and pyrazinamide may not be sufficiently effective. Apart from first burdening the patient with the side effects of toxic tuberculosis chemotherapy, the failure of the patient to adequately respond to the wrong treatment may prompt the treating clinician to apply even more toxic second-line anti-tuberculosis drugs, which, of course make the patient even more miserable without ridding him of Mycobacterium avium.
To treat or not to treat tuberculosis in elderly patients
Tuberculosis is an infectious disease. But most people who are infected never become ill with tuberculosis.
This limits the risk that people with active, contagious tuberculosis pose to their human environment.
By WHO estimates, one quarter of the world population of 8.1 billion, roughly 2 billion are infected.
However, 46 percent of all tuberculosis cases are concentrated in Southeast Asia.
About 8.5 percent of the world's population live in Southeast Asia.
If there is a proportional relationship between population numbers, active tuberculosis, and latent tuberculosis, one may well
assume that in Southeast Asia, pretty much everybody has latent tuberculosis.
The math goes like this. 10.5 million active tuberculosis cases per year are proportional to 2 billion people with a latent infection.
10.5 million times 46 percent is 4.83 million (the number of active cases in Southeast Asia).
2 billion times 46 percent is 920 million. That is the number of latent tuberculosis cases that would be equivalent to the 4.83 million active cases in Southeast Asia per year.
But the population of Southeast Asia is only 676 million. Thus one may as well assume that everybody in Southeast Asia has at least
latent tuberculosis.
About 1.5 million die each year of tuberculosis. The majority of those who die of, or with, tuberculosis are over 70 years of age.
The rest life expectancy of people aged 70 in 2024, with or without tuberculosis, isn't much.
Annuity tables, used primarily by insurance companies, calculate more than 10 years rest life expectancy for people in the US. The number may
be higher for Europe or Northeast Asia, but it is lower for most of the world.
However, the question for people 70 and over is not so much, how many years their hearts will keep on pumping. A more sensible evaluation is,
how much good time remains in store.
It's not a blessing to add years to one's life if those are years tainted by Alzheimer's, or bedridden years, or
years in chronic pain.
It's a blessing to die before it comes that far.
As mentioned previously, compared to younger populations, tuberculosis symptoms are often mild in the elderly (no fever, no night sweats,
no weight-loss, limited cough).
On the other hand, compared to younger populations, the side effects of tuberculosis chemotherapy are, in elderly populations, usually more severe
(daily nausea, stomach pain, joint pain, insomnia, new or aggravated kidney and liver disease, vision loss, hearing loss).
At the same time, even after having gone through the treatment torture for six or more months, the risk of a relapse of tuberculosis,
as measured by smear microscopy, is high. And then the treatment torture would start all over again, and at that time at a considerably
lower level of general health.
Thus, for people age 70 or older, who have active tuberculosis, albeit with bearable symptoms, it may just make sense to do nothing.
At age 70 or older, one will soon have to die of something anyway, and tuberculosis may just be the preferable lot, compared to
painful cancers. It may also be preferable to spending one's rest of life with crippling neurological disorders.
The question is whether the medical establishment, or the community, or even the family will allow an elderly person with tuberculosis
chose not to undergo treatment. There is reason to doubt it.
Tuberculosis and death
To wish for a gentle, even a comfortable death, is a legitimate concern.
Some people are not prepared to die, never. They want to extend their lives, by all medical or surgical means available, even when the time they gain is only suffering.
Sudden cardiac arrest is a gentle natural death. One may feel exhausted, then falls unconscious, and dies without being aware of it. It's a blessing.
Unless an ambulance comes and a paramedic messes things up, pulling a person back into life. That is a curse. And it should never happen.
Some deaths are gentle, like sudden cardiac arrest.
Other causes of deaths are extremely painful, like burning to death, and some are accompanied by extreme panic, like drowning.
Furthermore, the history of torture attests to just how much pain and suffering humans can inflict on other humans.
It would have been better not to have been born.
But while it may sound rational, to opt out by committing suicide in a comfortable manner, is not as easy as it sounds. Nature hasn't created us to just opt out. The closer one gets to taking action, the more reliably thoughts will be generated by the brain to undermine one's determination. Thoughts of hope, thoughts of what one does not want to miss, thoughts of what is unfinished in one's life.
So, better a natural death, like sudden cardiac arrest. Or how would that be: death from tuberculosis.
In the 17th and 18th century, death from tuberculosis was actually romanticized. It was described as a by-and-large painless fading away.
Here an example:
In Charlotte Brontë’s 1847 novel Jane Eyre, one of Jane’s classmates says “I am very happy, Jane; and when you hear that I am dead, you must be sure and not grieve; there is nothing to grieve about. We all must die one day, and the illness which is removing me is not painful; it is gentle and gradual; my mind is at rest.”
Extreme weakness appears to be a feature of advanced tuberculosis, with patients asleep for much of the day.
"The playwright’s wife, actress Olga Knipper-Chekhova, later remembered, 'He awoke in the early hours of the night, and for the first time in his life himself requested that the doctor be sent for.' When the German doctor arrived, 'Anton sat up unusually straight and said loudly and clearly in German (of which he knew very little): Ich sterbe (‘I’m dying’).' The doctor ordered a bottle of champagne be brought up. 'Anton took a full glass, examined it, smiled at me and said, ‘It’s a long time since I drank champagne.’ He drained it and lay quietly on his left side, and was soon silent forever.”
"In April 2017 Righetti’s team was given permission to analyze the relics from Chekhov’s final days, both to test the researchers’ methods against the playwright’s known tuberculosis diagnosis and to better understand the hour of his death... 'Our team was lucky, because fortunately we found traces of spittle and saliva and traces of blood, so we were able to identify the traces of tuberculosis,' says Zilberstein.
And the team found something else. Among the protein markers in the sample they found a protein known as ITIH4, which is produced in response to blood clots. This suggests that the immediate cause of Chekhov’s death was not heart failure or suffocation caused by the infection itself but a stroke, which cut off blood supply to an artery in the writer’s brain."
The misguided WHO End Tuberculosis strategy
In May 2014, the World Health Assembly of the United Nations commissioned the WHO to reduce (compared the 2015 numbers) tuberculosis death by 95 percent, and the incidence of active tuberculosis by 90 percent. Timeframe: these goals are to be achieved by 2035.
And the WHO has since been waging a mainly pharmaceutical war against Mycobacterium tuberculosis.
The WHO estimates that roughly a quarter of the world's 8 billion people have latent TB. They carry the pathogen but have no symptoms. More than 90 percent of those with latent tuberculosis will die of other causes without their health ever having been compromised by the pathogen, and without ever having been contagious.
Nevertheless, the WHO recommends toxic chemotherapy of several months even for latent tuberculosis.
But the WHO strategy is flawed because tuberculosis depends heavily on environmental factors. This was initially postulated more than 70 years ago, ironically by a scientist who developed antibiotica: The French-American microbiologist René Dubos
Polluted air is possibly the single most important factor that turns latent tuberculosis into active disease.
Between 1850 and 1950, tuberculosis declined steadily in Western Europe at substantial margins, not because effective drug therapies would have been available but because living conditions improved, and populations developed a general awareness of the importance of clean air in order to contain tuberculosis.
Relevant as air pollution may be, it's probably not the only factor.
And rather than sniffing out latent tuberculosis cases, and applying the chemotherapy hammer to bacilli hidden deep in granulomas, the WHO should use some of its funds for epidemiological research on what else, apart from air pollution, turns latent tuberculosis into active disease, and how this can be avoided.
To reduce the annual rates of the conversion from latent to active tuberculosis by campaigning against air pollution may be the easier task, compared to feeding toxic pills to people who may have tuberculosis but no symptoms.
And if money is spent on epidemiological research, there may even be some easy solutions to a complicated problem, as a Singaporean epidemiologic study suggests. The scientists found out that in Singapore, people who drank tea reduced their risk of having their latent tuberculosis go active by 18 percent.
Tuberculosis and fresh air
The idea that fresh air treats and possibly cures tuberculosis, is old.
"Hippocrates (460 B. C.), “the Father of Medicine,” used sunlight in treating tuberculosis; in fact, he used what appears to be a very modern
treatment for this disease, since he recommended that the sufferer be sent away to the hills beyond the city, where he would have plenty
of rest, fresh air and sunshine."
In Europe, tuberculosis was especially bad between the mid-18th and early 19th century during the industrial revolution. People moved
from the countryside to rapidly growing cities where they lived in poor, crammed conditions, and were exposed to heavy pollution
from the burning of coal.
From the mid-19th century, anywhere in Europe and North America, a "new" kind of knowledge spread quickly: that fresh air is a necessity,
both to avoid tuberculosis, and to treat and potentially cure it.
The first protagonist of this idea was the German physician Herman Brehmer who cured his own tuberculosis in the Himalayas.
"The first German sanatorium for the systematic open-air treatment had been started by Hermann Brehmer (1826-1889) at Görbersdorf in
Silesia in 1854... The results were regarded as highly successful, surpassing any previous treatment... Mander Smyth described the
regimen at Nordrach, where he experienced it as a patient and subsequently practiced it as an assistant to Walther. The first
component was fresh air, both by day (out of doors if possible) and by night with wide-open windows. Rest was the next
important factor, in bed initially... Rest included mental rest, with protection from visitors and from talkative neighbors.
When... the doctor was satisfied with progress, exercise could start... Walking began with short distances at a controlled
pace avoiding breathlessness; ultimately it would be many miles in a day. The diet was abundant..."
Sanatoria were opened throughout Western Europe and North America. But not only that.
In North America, patients who could not afford sanatoria but had enough money for long-distance public transport, traveled and
resettled in large numbers to places where the climate was less polluted, like Colorado and Arizona.
The original location of the clip is:
Public health programs and city planning incorporated the awareness of the necessity of fresh air and nature, though it takes
decades from awareness to implementation.
"What Tuberculosis did for Modernism: The Influence of a Curative Environment on Modernist Design and Architecture"
The influential 1952 book The White Plague: Tuberculosis, Man and Society, written by the famed French-American microbiologist
René Dubos and his wife Jean Dubos, summarized the fresh air / green space narrative, claiming that basically,
tuberculosis is an environmental and social disease, caused by unsavory, crammed living conditions with high levels
of air pollution and poor nutrition. The authors credited social improvements rather than the medical profession
for the marked decline in the number of tuberculosis cases and deaths between the mid-19th and mid-20th, even before the
advent of tuberculosis chemotherapy.
While the exact impact of fresh air on the healing of active tuberculosis may be harder to ascertain, many scientific studies
have proven that lungs that are stressed by voluntary or involuntary inhalation of smoke and many kinds of air pollution are
more susceptible to tuberculosis disease.
"Cigarette smoke (CS) exposure is a key risk factor for both active and latent tuberculosis (TB). It is associated with delayed
diagnosis, more severe disease progression, unfavorable treatment outcomes and relapse after treatment."
In many low and mid-income countries in tropical parts of the world, especially in Southeast Asia, South Asia, and
Africa, solid biomass fuel like wood or charcoal are used for cooking and heating. Household trash and
agricultural waste are often burned before every house, or in the vicinity of communities.
Many studies have confirmed that these patterns are associated with high incidence rates for tuberculosis.
"Biomass smoke is a significant risk factor for active tuberculosis."
Environmental pollution, caused by industrial activities and fossil fuels, likewise causes increases in tuberculosis.
A 2023 Chinese study of 14.8 million tuberculosis cases between 2004 and 2018 found that a high degree of PM2.5 pollution
(93.3–145.0 micrograms /cubic meter of air) more than doubled active tuberculosis cases, compared to low PM2.5 pollution. Tuberculosis and bed rest
Up until the mid-20th century, bed rest was the most promising treatment for tuberculosis.
Patients, especially those from families of sufficient wealth, stayed for months or years at sanatoria where they passed their days in
tranquil natural environments, hanging around on sofas on balconies, or, if febrile, lying in bed.
"In Europe, the first sanatorium was founded in 1854 by Hermann Brehmer in Germany, in Goebersdorf in Silesia, a village on the border
between Poland and the Czech Republic... His method of treatment spread throughout Germany, France and Switzerland, especially in the
egion of Davos, in the Engadin Valley, where the first high-altitude sanatoria were opened for paying patients...
The new sanatoria were designed in such a way that patients could stay in single rooms or rooms with a few beds,
which usually gave onto large terraces where inmates could take so-called “sun baths”.
The buildings were surrounded by spacious meadows and tree-lined gardens, where guests could go for long healthy walks.
Patients stayed in the institution for very long periods – from a minimum of six months to seven, eight or even 16 years."
"It wasn't until the development of the Sanatorium in which careful observations were made... that the rest cure came into the foreground
as the most important factor in combating the disease. “Rest” is the most important single factor in the treatment of pulmonary
tuberculosis. - Chest Journal, January 1942, Rest in Treatment of Tuberculosis by Savere Madonna, MD
But just when discoveries were made on why bed rest sometimes was successful, and how it could be optimized, along came the discovery
of streptomycin and other agents of chemotherapy which were way more economical than sanatoria and more reliable in treating the disease,
albeit at the cost of substantial systemic side effects.
The proposed optimization of bed rest (in which mainstream medicine was no longer interested) was based on a better understanding of lung physiology.
"The purpose of this review is to re-examine the physiologic evidence pertaining to these treatments [bed rest, pneumothorax] and to emphasize why we
should have listened to one man, William (Bill) Dock, who told us all long ago how bed rest should be performed and why certain types of
collapse might be helpful.
It is an established observation in the diagnosis of pulmonary tuberculosis that the bacilli have a preference for the upper one third, and even
the apices of the lungs.
"What could possibly explain these... preferences?... The answer was finally provided by Bill Dock... who came up with a very simple
explanation...: gravity, which has important effects on both the distribution of inspired air and the distribution of pulmonary arterial
blood flow within the lungs."
Mycobacterium tuberculosis is an obligate aerobe. It needs oxygen to thrive, the more the better.
The availability of oxygen to the bacilli isn't uniform in the normal human lungs. In the upright position, in which people find themselves for
most of the day when standing, walking, or sitting, gravity causes the bases of the lungs to receive the most blood supply, and this is
where most gas exchange takes place.
Normal tidal breathing involves only 1 to 2 liters of air per breath, while the full lungs volume of the average
person is 5 to 6 liters.
When only 1 to 2 liters of air are used in gas exchange in about one third of the lungs, the remaining capacities of the lungs are not empty.
They also contain air, mostly oxygen-rich.
One such part of each lung which is filled with air that participates little in gas exchange is the upper lobe, especially the apex.
"Very little of the total oxygen uptake occurs at the apex, principally because the blood flow there is very low... Note that the base of the
lung has most of the blood flow, but the PO2 [oxygen tension, oxygen pressure] and oxygen concentration of the end-capillary blood are lowest
there. As a result, the effluent pulmonary venous blood (which becomes the systemic arterial blood) is loaded with moderately
oxygenated blood from the base."
In people who go about their lives in a normal manner, with the lungs upright for most of the day, the upper lobes present an ideal
environment for the bacilli. They contain oxygen-rich air which, because of the effects of gravity on blood flow in the pulmonary circulation,
is largely unaffected by the fluctuations of gas exchange.
And the forces of gravity in the erect human host work in favor of the bacilli not only because of stable oxygen-rich air pockets,
but also by shielding the bacilli from a full-blown attack by the host immune system. Not only the flow of blood to the apices of the
lungs is hampered in the upright position, but even more so the flow of lymph.
All of this can be reversed by positional intervention. When a human host is lying flat on his or her back, then, all of a sudden,
the apices of the lungs are no longer a haven of oxygen-rich air with little gas exchange. On the contrary, the apices are now, because of
gravity, an area of intense blood flow and gas exchange. Furthermore, also because of gravity, the immune system, via lymph, has a new tactical
advantage over the pathogen.
Bed rest, it must be noted, is most effective if a person lies flat on his back. But many by-and-large healthy people, and most people
confined to hospital beds for any kind of disease, do not lie flat. They pop up their upper torsos with pillows, or adjust their
hospital beds to up to 45 degree. This may be fine for many diseases, and even beneficial for GERD (gastroesophageal reflux disease)
but negates the desired end points in the case of tuberculosis.
As many historical images of patients in sanatoria prove, bed rest was often done wrong, with upper torsos elevated.
This surely was comfortable, not only for the human hosts but also for the bacilli.
An excellent summary on the importance of body position was provided by Scott Welker MD at an unlikely Internet
location, Quora:
"Rest therapy for TB works mainly because of the position of the patient when they are at rest. Partly because of reduced stress on the immune
system and cleaner air also, but mainly it was that laying down deprived the TB of oxygen.
"The Mycobacterium tuberculosis organism is a strict aerobe, and it thrives in environments with excess oxygen. The opposite is also true - deprive it of oxygen, and it fares poorly.
"To explain this I first need to explain pulmonary physiology. Obviously we have a large pulmonary reserve. That’s why you can breathe
hard enough to run, or work hard, of row a boat. Your lungs can support much greater exertion than you are experiencing right now.
A healthy adult can even get by after an entire lung is removed!
"At rest, we only need about 1/3 of the capacity of our lungs. Oxygen exchange takes place mainly in the middle third, as the bottom third of
the lungs are congested by blood flow and not well aerated. The top third is well aerated, but only gets enough blood flow for the lung itself;
very little blood flows into the oxygen-exchange vessels. So that’s one of the reasons TB favors the upper 1/3 of the lung; there’s tons of
oxygen there that’s not being used. We inhale it, then exhale it without absorbing it... Here’s a cartoon I drew to illustrate this:
"So, when you lie in a bed, you’re still only using the middle 1/3 of your lung for oxygen exchange. same situation as when you’re standing,
but now your lung is horizontal. The top 1/3 faces the ceiling, and the bottom 1/3 faces the floor. The slices of the sandwich still go
90 degrees to up and down, but some or all of the M. tuberculosis colony in the chest is either struggling with less oxygen
(which exchanged in your lungs’ middle 1/3), or getting no oxygen at all (it’s submerged in your lungs’ bottom 1/3).
"In his brilliant 1934 Textbook of Medicine, Dr. Russel B. Cecil pointed this out. Even though we hadn’t figured out the 'lung in thirds' model
I speak of above, because we lacked the equipment to take blood pressures in the pulmonary veins and do nuclear medicine perfusion scans,
Cecil deduced the truth of this. He said 'rest is the only treatment which has proved entirely successful.' He went on to point out that
patients who had disease on one side of their chest only (which we could see on X-rays and bronchoscopy), were better served to lie with
their diseased lung down.
"He even forbid patients from 'sitting up in a chair or reclining in a chaise-lounge.' ... So there you have it - rest worked for TB because
it deprived the organism of oxygen.
Tuberculosis and high altitude
Being at high altitudes slows tuberculosis progression, and improves the odds of self-cure. This was observed in the
pre-chemotherapy era, and it has been confirmed in recent scientific research. The following is from a 2013 study.
"Antimycobacterial immunity was assayed in 15 healthy adults residing at low altitude before and after they ascended to 3400 meters,
and in 47 long-term high-altitude residents. Antimycobacterial immunity was assessed as the extent to
which participants’ whole blood supported or restricted growth of genetically modified luminescent Bacille Calmette-Guérin, (BCG),
mycobacteria during 96 hours incubation... At low altitude, mycobacteria grew in blood 25-times more than in negative-control plasma,
whereas ascent to high altitude was associated with restriction of mycobacterial growth to be only 6-times more than in [negative-control] plasma.
There was no evidence of differences in antimycobacterial immunity at high altitude between people who had recently ascended to high altitude,
versus long-term high-altitude residents."
The above matches scientific research that has been conducted in the pre-chemotherapy era, summarized in 2013 in a
scientific article under the headline "Tuberculosis and High Altitude. Worth a Try in Extensively Drug-Resistant Tuberculosis?"
"In 1925, for example, the experiments of Novy and Soule on the 'Respiration of the Tubercle Bacillus' showed that
higher than usual ambient oxygen concentrations... enhanced bacillary growth... By contrast, exposure to lower than normal oxygen concentrations
showed 'for the first time' that growth 'decreased progressively as the [oxygen] tension was lowered'; 2 years later, the experiments of
Corper, Lurie, and Uyei came to nearly similar conclusions about the effects of low oxygen tensions. Then, in 1939, Kempner
determined that the rate of oxygen utilization of cultured tubercle bacilli decreased in curvilinear fashion as the oxygen percentage of
exposed bacilli was reduced."
In the late 19th and early 20th century, it was common knowledge that higher altitudes afforded a window of opportunity
against tuberculosis.
"When John Henry “Doc” Holliday headed to Denver, Colorado, in 1882, he was escaping murder charges for his
involvement in a shootout at the O.K. Corral. But he stayed in the state... for the sake of his lungs. Holliday suffered from
tuberculosis, and at the time everyone knew that Colorado was the best place for so-called “lungers” to rest and recover...
Physicians in the 19th and 20th centuries believed that fresh air, high altitudes and abundant sunshine could cure all kinds of ailments,
and Colorado had plenty of all three. Although their beliefs about TB were not entirely medically sound, they were kind of right in
this regard: Fresh air does prevent TB from spreading, and the high altitude stops TB bacteria from spreading rapidly through the lungs...
Beginning in the 1860s, ill people began pouring into the future state to take the fresh air cure. Denver’s first facility for tubercular
patients was built in 1860, just two years after the city was founded."
"The introduction of the sanatorium cure provided the first real step against TB. Hermann Brehmer, a Silesian botany student
suffering from TB, was instructed by his doctor to seek out a healthier climate. He traveled to the Himalayan Mountains where he could
pursue his botanical studies while trying to rid himself of the disease. He returned home cured and began to study medicine.
In 1854, he presented his doctoral dissertation bearing the auspicious title, Tuberculosis is a Curable Disease. In the same year,
he built an institution in Goebersdorf where, in the midst of fir trees, and with good nutrition, patients were exposed on their balconies to
continuous fresh air. This setup became the blueprint for the subsequent development of sanatoria, a powerful weapon in the battle against
an insidious opponent."
"The global prevalence of multidrug-resistant, mono drug-resistant, isoniazid[-resitant], and rifampicin[-resistant] tuberculosis are
11.6%, 11.8%, 15.7%, and 9.4%, respectively.
Feeding patients with toxic antibiotics to which the bacteria are resistant only produces additional morbidities, without reducing
the Mycobaterium tuberculosis load. In all likelihood, these additional morbidities reduce the chance of self-cure, which, with the right
supportive measures can be as high as 50 percent. (See the paragraphs on "Untreated tuberculosis".)
The world's foremost scientific journal, Nature, in 2014: "Curiously, in recent years some ‘old solutions’ were also proposed
to contrast drug-resistant strains, such as the establishment of sanatorium-like structures for admission of incurable cases."
"Incurable cases" in the Nature article means: cases that cannot be cured by chemotherapy. But even before chemotherapy was
invented, a certain percentage of patients won the battle against tuberculosis, either via "mysterious" self-cure, or with an
appropriate care that did not include medications. The chances in sanatoria were better than at home.
Tuberculosis, a nutritional disease
It has long been assumed that tuberculosis is a social disease that affects mostly poor, malnourished people who live in places with highly polluted air, indoors and outdoors.
But this observation is not specific enough. Not only do some better-to-do people also fall ill with active tuberculosis; even among poor people in the poorest countries, the vast majority does not get tuberculosis. The incidence rate of active tuberculosis, even in the worst affected countries, is less than 1 percent.
Sure, if one visits tuberculosis patients in communities, a large number of them will be malnourished. If they weren't already malnourished when they fell I'll with tuberculosis, then the disease will likely make them malnourished.
There clearly is a correlation between nutrition and tuberculosis, but it's not primarily that poor people get the disease.
Rather, tuberculosis mostly strikes people who are thin (even when they are rich), and people who eat no meat (not because they could not afford it, but for religious or ideological reasons).
"In a study among 1,717,655 Norwegians, >15-years old who were followed for 8–19 years after intake into a radiographic screening program, the relative risk of tuberculosis among persons in the lowest body mass index (BMI) category was more than five-fold higher than the group in the highest BMI category... In another study conducted in London, it was found that Hindu Asians had an increased risk of tuberculosis compared with Muslims. Religion had no independent influence after adjustment for vegetarianism (common among Hindu Asians). There was a trend of increasing risk of tuberculosis with decreasing frequency of meat or fish consumption. Lacto-vegetarians had an 8.5-fold risk compared with daily meat/fish eaters."
People who are underweight, either by choice or because they do not have enough money to buy food, are more prone to fall ill with tuberculosis than overweight or obese people. This is an established fact, proven in epidemiological studies.
Why are thin people more likely to fall I'll with tuberculosis?
Here some biochemical speculation that may or may not be true.
It could be because of the hormone leptin.
Leptin is synthesized in adipocytes (fat cells). The more adipocytes, the more leptin.
Leptin affects immune cells, directing them towards inflammation. This is often unwanted, but not in the case of tuberculosis when leptin apparently is part of a successful immune defense, hindering latent tuberculosis from becoming active.
While there is good evidence that a higher BMI protects against tuberculosis disease, it would be interesting to know how weight gain affects tuberculosis healing.
Indeed, weight gain in chemotherapy-treated tuberculosis is associated with improved outcomes.
And when the sanatorium movement started in the mid-19th century, fresh air was just one of two treatment pillars; the other, no less important, was sumptuous meals. And combined, these two prescriptions achieved noticeable cure rates.
The traditional name for tuberculosis is "consumption". The wasting in tuberculosis doesn't just happen because people are ill. Rather, it is the result of a willful, skillful manipulation of the host's metabolism by Mycobacterium tuberculosis, designed to undermine the host's immune response for the sole purpose of the survival and propagation of the bacterium.
How to react as a tuberculosis patient? Eat! Eat some meat! Overeat! Gain weight! Worry about obesity-related diseases after you are done with tuberculosis.
Tuberculosis and inflammation
Inflammation is at the core of the immune system.
"If you don't have inflammation, then you'll die," Ed Rainger, a professor who studies chronic inflammation at the University of Birmingham in the U.K., told Live Science. "It's as simple as that."
Inflammation is a complex process, involving multiple immune cells and numerous molecules, like cytokines, that regulate it.
Inflammatory cytokines defend the body against pathogens, including Mycobacterium tuberculosis.
"Multiple host immune factors control the formation of a self-organizing aggregate of immune cells termed a granuloma in the lungs after inhalation of Mtb. One such factor, tumor necrosis factor-α (TNF), is a protein that regulates inflammatory immune responses. Availability of TNF within a TB granuloma has been proposed to have a critical role in the protective immunity against TB."
As a treatment option for autoimmune diseases, the pharmaceutical industry has developed tumor necrosis factor inhibitors. A sorry side effect of TNF inhibitors is that in patients using them, a latent tuberculosis infection may become active tuberculosis disease.
"Tumour necrosis factor (TNF) is a potent inflammatory cytokine that plays an important role in immunity to numerous bacterial infections, including Mycobacterium tuberculosis (Mtb), the causative agent of tuberculosis (TB) in humans. [Some drugs] are anti-TNF agents used to treat a range of inflammatory / autoimmune diseases, such as rheumatoid arthritis. The use of some of these drugs has been linked to reactivation TB."
A key tool of Mycobacterium tuberculosis in making immune cells their survival niche is the down-regulation of pro-inflammatory cytokines like TNF (tumor necrosis factor).
"M. tuberculosis can evade antituberculosis (anti-TB) immunity by inhibiting host cell TNF production via expression of specific mycobacterial components."
If a lack of tumor necrosis factor favors Mycobacterium tuberculosis, would enhancing tumor necrosis factor heal the disease?
Mind you, theory is a physician with a poor track record. There is no clinical or epidemiological evidence that interventions that enhance tumor necrosis factor-driven inflammation would get rid of tuberculosis, or even just ameliorate the condition.
Epidemiological data rather the opposite. When young adults with strong immune systems suffer from active tuberculosis, they often become violently ill.
On the contrary, in elderly patients with age-related weaker immune systems, active tuberculosis often presents with fewer, or few, clinical symptoms.
"Typical pulmonary TB symptoms such as prolonged cough, haemoptysis, night sweats, chills, fatigue, and loss of appetite are less prominent in older adults with TB... Radiological features also differ between younger and older adults, with older adults less likely to have lung nodules or consolidation on computed tomography (CT) or typical apical lung cavities on the chest radiograph. The presence of lung nodules and soft tissue masses is also more likely to indicate malignancies in older adults, which may co-exist with TB disease."
At some point in the progress of tuberculosis, matters get turned around. At an early stage after infection, a strong immune system can contain Mycobacterium tuberculosis in isolated granulomas.
But when that fails, a strong immune response makes matters worse for the human host by causing cavities in the lung tissue, which favor the pathogen.
"During active TB, pro-inflammatory immune responses are often robust but fail to contain bacterial proliferation, leading to tissue damage and non-productive inflammation. Adjunctive TB HDT [host-directed therapy] treatment aims avoid the development of irreversible lung damage from non-productive inflammatory responses to thereby improve the quality of life of TB survivors." Tuberculosis and turmeric
Turmeric reduces the frequency and intensity of coughing in patients with tuberculosis.
This is a simple observation that is easy to verify by anybody who either is a tuberculosis patient or takes care of one.
This does not mean that turmeric cures tuberculosis.
Turmeric is a spice used in curries. No problem is associated with consuming around 10 grams a day. Anyway, the active ingredients, which includes curcumin, are poorly absorbed.
Double-blind placebo-controlled clinical trials are the gold standard when testing pharmacological and medical interventions.Turmeric and isolates have been amazingly well researched in such studies.
A 2023 review:
"Eight databases were searched using established guidelines, yielding 389 citations (from 9528 initial) that met inclusion criteria. Half focused on obesity-associated metabolic disorders (29%) or musculoskeletal disorders (17%), where inflammation is a key driver, and beneficial effects on clinical outcomes and/or biomarkers were reported for most citations (75%) in studies that were primarily double-blind, randomized, and placebo-controlled trials (77%, D-RCT). Citations for the next most studied disease categories (neurocognitive [11%] or gastrointestinal disorders [10%], or cancer [9%]), were far fewer in number and yielded mixed results depending on study quality and condition studied. Although additional research is needed, including systematic evaluation of diverse curcumin formulations and doses in larger D-RCT studies, the preponderance of current evidence for several highly studied diseases (e.g., metabolic syndrome, osteoarthritis), which are also clinically common, are suggestive of clinical benefits."
The evidence is strongest for the treatment of inflammatory diseases.
"Curcuma or its derivatives can be used safely and efficiently as adjuvants or as a main therapy for these diseases [Inflammatory Bowel Disease, Osteoarthritis, Systemic Lupus Erythematous, Psoriasis, and Sclerosis]"
"Curcumin inhibits these autoimmune diseases by regulating inflammatory cytokines such as IL-1beta, IL-6, IL-12, TNF-alpha and IFN-gamma and associated JAK-STAT, AP-1, and NF-kappaB signaling pathways in immune cells."
One pioneering US study examined curcumin for tuberculosis.
"We found that curcumin enhanced the clearance of MTB [Mycobacterium tuberculosis] in differentiated THP-1 human monocytes and in primary human alveolar macrophages. We also found that curcumin was an inducer of caspase-3-dependent apoptosis and autophagy. Curcumin mediated these anti-MTB cellular functions, in part, via inhibition of nuclear factor-kappa B activation."
"Caspase-3 is one of the members of the family of caspases (cysteine-aspartic-proteases) which are proteolytic enzymes known for their key roles in apoptosis."
Apoptosis involves the controlled extermination of bacteria, even cancer cells, within macrophages. If apoptosis of Mycobacteria tuberculosis-infected macrophages could be induced by turmeric on a large scale, this would surely be a victory.
Unfortunately, the above-quoted study on tuberculosis and turmeric was only done in vitro, on human cells in lab dishes. The results of in vitro studies can often not be replicated in vivo, living organisms, animals or humans.
A 2022 in vivo study found:
"Previous experiments found that the substantial pulmonary inflammation associated with TB causes neuroinflammation, neuronal death, and behavioral impairments in the absence of brain infection. Curcumin (CUR) is a natural product with antioxidant, anti-inflammatory and antibacterial activities. In this work, we evaluated the CUR effect on the growth control of mycobacteria in the lungs and the anti-inflammatory effect in the brain using a model of progressive pulmonary TB in BALB/c mice infected with drug-sensitive mycobacteria (strain H37Rv). The results have shown that CUR decreased lung bacilli load and pneumonia of infected animals. Finally, CUR significantly decreased neuroinflammation (expression of TNFα [tumor necrosis factor alpha], IFNγ [interferon-gamma] and IL12 [interleukin-12]) and slightly increased the levels of nuclear factor erythroid 2-related to factor 2 (Nrf2) and the brain-derived neurotrophic factor (BDNF) levels, improving behavioral status. These results suggest that CUR has a bactericidal effect and can control pulmonary mycobacterial infection and reduce neuroinflammation."
Interestingly, the above study addressed the often neglected issue of tuberculosis-induced chronic inflammation involving the brain. That turmeric ameliorates, albeit in mice, tuberculosis-related brain inflammation is in line with human double-blind placebo-controlled clinical trials that have proven the anti-inflammatory power of turmeric.
Tuberculosis and vitamin D
A number of studies have shown that tuberculosis is associated with low vitamin D status.
"A case-control study was conducted in a tertiary care hospital from 2014 to 2016, including 50 adult newly diagnosed sputum positive pulmonary tuberculosis patients... and 50 age and sex-matched healthy participants as control group. Results: In both groups, the majority were men (88%). BMI was significantly lower in the tuberculosis group (19.40 (17.20, 22.0) vs. 24.00 (22.50, 25.47)). Serum vitamin D levels were significantly lower in the tuberculosis group (19 (7.75, 27.25) ng/dl) as compared to the control group (25 (19.75, 32.00) ng/dl). Out of 50 TB patients, 27 (54%) had vitamin D deficiency, while among healthy controls, only 13 (26%) had vitamin D deficiency. Among vitamin D deficient PTB [pulmonary tuberculosis] patients, 44% had 3+/hpf AFB in sputum smear examination. Conclusion: The prevalence of vitamin D deficiency in pulmonary tuberculosis cases is very high. Hypovitaminosis D was associated with more severe clinical symptoms, higher sputum smear positivity, and extensive lesions in chest radiographs."
The value "3+/hpf AFB" in the above quote refers to the number of bacteria discovered in sputum during a microscopic examination.
"Reading smears is a critical step in sputum microscopy. The Global Laboratory Initiative (GLI) handbook for acid-fast microscopy specifies guidelines for reading, recording, and reporting results for both, Ziehl-Neelsen and the auramine methods.
When Mycobacteria tuberculosis invade the human body through the lungs, they are (just like any other bacteria) ingested by macrophages. Inside the macrophages, the bacteria are then concentrated in organelles called phagosomes.
A healthy process would be for phagosomes to fuse with lysosomes, another organelle. Then, aggressive chemicals in the lysosomes kill the bacteria.
But something goes wrong when the pathogen is Mycobacteria tuberculosis. Once in the phagosome, Mycobacterium tuberculosis secretes molecules that hinder the fusion of phagosomes with lysosomes, and thus, the mycobacteria stay alive and duplicate.
Sooner or later, the Mycobacterium tuberculosis-infected macrophages die a chaotic death in which their cell walls burst. This kind of cell death is called necrosis. In necrosis, the mycobacteria break free and are ingested by other nearby macrophages. This is one way, tuberculosis spreads through the host organism.
There is another kind of cell death, called apoptosis (programmed cell death). This would occur if phagosomes and lysosomes inside the macrophages could fuse, and the mycobacteria would be killed in these phago-lysosomes, and the cell would die when exhausted by this innate immune function.
This kind of cell death, apoptosis, would release live bacteria into its neighborhood, and would not have detrimental effects like necrosis.
How Mycobacterium tuberculosis obstructs the fusion of phagosomes with lysosomes, has been the subject of intensive research.
Two potential pathways have emerged. One involves the intracellular enzyme caspase-3, which controls apoptosis. The other is about a protein in the coating of phagosomes, called TACO (tryptophan-aspartate containing coat protein).
There is much more TACO in the coats of phagosomes that have accumulated Mycobacteria tuberculosis than there should be. And it's not that Mycobacteria tuberculosis would make this protein. Rather, it is a protein encoded in the human genome, and Mycobacteria tuberculosis just disseminate signal molecules that cause macrophages to overly express the gene for TACO.
This already is cell biochemistry at an astonishingly deep level.
Now, put vitamin D into the mix. Vitamin D apparently has the capability to interfere with the complicated mechanism of how Mycobacteria tuberculosis cause TACO over-expression in phagosome coatings.
"Recently, gene coding for tryptophan-aspartate containing coat protein (TACO) has been recognized to play a crucial role in the survival of Mycobacterium tuberculosis within human macrophages. Since regulation of the TACO gene is still poorly understood, the present study was addressed to explore the role of vitamins (A, C, D, and E) in TACO gene transcription. Such a study revealed that synergistic action of vitamin D3 and retinoic acid (RA) had the inherent ability to down-regulate TACO gene transcription in human macrophages. Based upon these results, we propose that the synergistic action of RA + vitamin D may be of importance in the prevention/control of M. tuberculosis infection."
Retinoic acid (RA) is a metabolite of vitamin A.
Tuberculosis and vitamin C
Practitioners of orthomolecular medicine believe that megadoses of vitamin C can keep any infection in check, and tuberculosis is not excluded from the claim.
By tongkatali.org
tongkataliorg3@gmail.com
Updated August 11, 2024
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3982203/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC8663960/
https://reviews.webmd.com/drugs/
drugreview-1744
-rifampin-oral
or
https://www.drugs.com/comments/
rifampin/?search=&sort_reviews=
lowest_rating#reviews
https://reviews.webmd.com/
drugs/drugreview
-8665-isoniazid-oral
or
https://www.drugs.com/comments/
isoniazid/?search=&sort_reviews=
lowest_rating#reviews
https://www.mayoclinicproceedings.org/
article/S0025-6196(11)62721-3/fulltext
https://eyewiki.aao.org/Ethambutol_Optic
_Neuropathy
https://bmcearnosethroatdisord.
biomedcentral.com/
articles/10.1186/1472-6815-7-5
https://www.sciencedirect.com/
science/article/
pii/S2405579421000188
https://pubmed.ncbi.nlm.nih.gov/
30333388/
https://pubmed.ncbi.nlm.
nih.gov/25352683/
https://bmcmedicine.biomedcentral.
com/articles/10.1186/
s12916-018-1033-7
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC2647396/
https://bmcmedethics.biomedcentral.
com/articles/
10.1186/1472-6939-14-25
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4448591/
https://en.wikipedia.org/wiki/
Medecins_Sans_Frontieres
https://www.sciencedirect.com/topics/
medicine-and-
dentistry/bedaquiline
https://erj.ersjournals.com/
content/25/3/564
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC6360468/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4663856/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3346619/
https://www.nature.com/
articles/s41579-022-00763-4
https://www.nature.com/
articles/nrd.2017.162
https://pubmed.ncbi.nlm.
nih.gov/27012592/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3070694/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC10443783
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC10443783
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4258661/
https://pubmed.ncbi.nlm.nih.gov/
25790407/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4937760/
https://www.thelancet.com/journals/lanres/
article/PIIS2213-2600(23)00097-8/abstract
https://www.thelancet.com/
journals/laninf/
article/PIIS1473-3099(24)00011-2/abstract
https://www.who.int/teams/global-tuberculosis-programme/
tb-reports/global-tuberculosis-report-2023/
tb-disease-burden/1-1-tb-incidence
https://data.worldbank.org/indicator/
SH.TBS.INCD
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC10443783
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC8753649/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC8703289/
https://www.sciencedirect.com/science/
article/pii/S120197121401707X
https://openres.ersjournals.com/
content/erjor
/5/4/00228-2018.full.pdf
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3217998/
https://pmc.ncbi.nlm.nih.gov/
articles/PMC7566660/
https://openres.ersjournals.com/
content/erjor/5/4/00228-2018.
full.pdf
https://pmc.ncbi.nlm.nih.gov/
articles/PMC7469952/
https://publications.ersnet.org/
content/errev/31/163/210212
https://www.who.int/teams/global-tuberculosis-programme/
tb-reports/global-tuberculosis-report-2023/
tb-disease-burden/1-1-tb-incidence
https://en.m.wikipedia.org/wiki/
Southeast_Asia
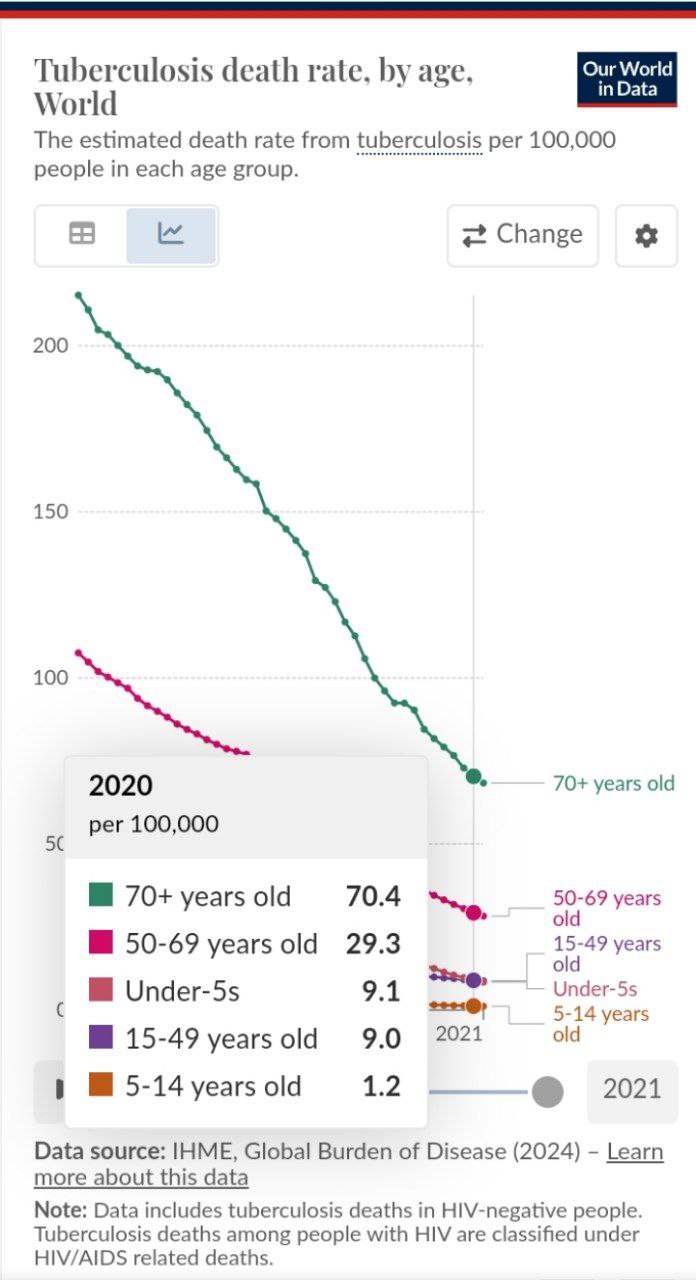
https://www.annuityadvantage.com/
resources/life-expectancy-tables/

https://www.who.int/teams/
global-tuberculosis-programme/
the-end-tb-strategy
https://www.who.int/publications/
i/item/9789241548908
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC5490523
https://journal.chestnet.org/
article/S0096-0217(16)30299-0/abstract
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC1281640/
https://www.pbs.org/wgbh/
americanexperience/features/
plague-chapter1/
https://www.cambridge.org/core/journals/
medical-history/article/what-tuberculosis-did-
for-modernism-the-influence-of-a-curative
-environment-on-modernist-design-
and-architecture/
https://err.ersjournals.com/content/
31/164/210252
https://jech.bmj.com/
content/68/12/1112
https://www.researchgate.net/
publication/37288971_Association_of_
air_pollutants_and_meteorological_
factors_with_tuberculosis_
a_national_multicenter_
ecological_study_in_China
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC6319124/
journal.chestnet.org/
article/S0096-0217(15)30204-1/abstract
https://www.atsjournals.org/doi/full/
10.1164/rccm.200307-1016OE
https://www.atsjournals.org/doi/full/
10.1164/rccm.200307-1016OE
https://www.sciencedirect.com/topics/
immunology-and-microbiology/lung-gas-exchange

Mont Alto Sanatorium in Pennsylvania, USA

Stannington, UK, Children's Sanatorium, 1926
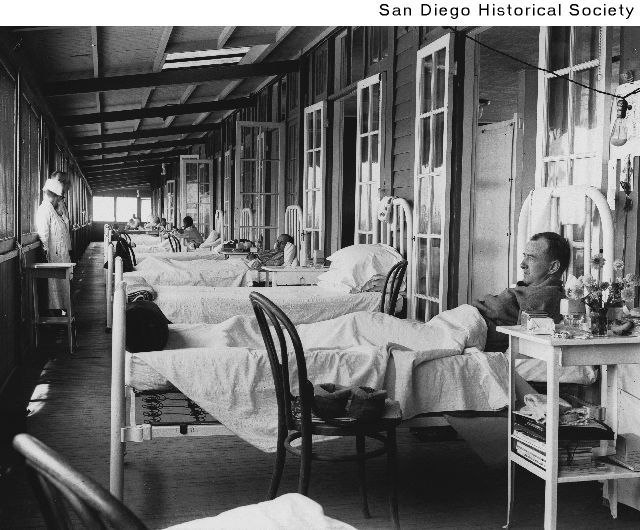
A ward at the Vauclain Tuberculosis Sanatorium, ca. 1920
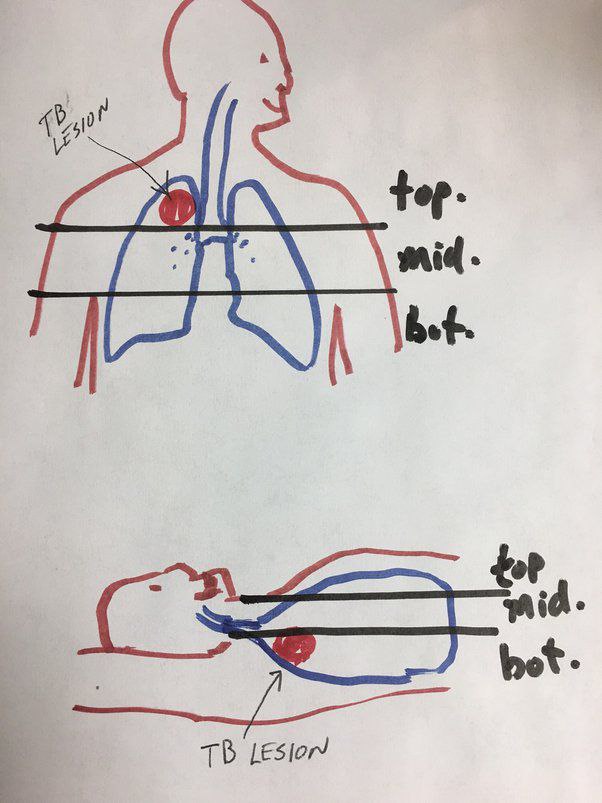
https://www.quora.com/Was-fresh-air
-and-lots-of-rest-ever-a-genuinely-effective-
treatment-for-some-tuberculosis-patients
https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC3772817/
https://www.atsjournals.org/doi/
full/10.1164/rccm.201311-2043OE
https://www.history.com/news/the-
disease-that-helped-put-colorado-on-the-map
https://globaltb.njms.rutgers.edu/
abouttb/historyoftb.php
https://idpjournal.biomedcentral.com/
articles/10.1186/s40249-023-01107-x
https://www.nature.com/
articles/ja2014108#ref-CR36e
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC2813110/
https://www.livescience.com/health/
immune-system/if-you-dont-have-
inflammation-then-youll-die-how-
scientists-are-reprogramming-the-bodys-natural-
superpower
https://journals.plos.org/ploscompbiol/
article?id=10.1371/journal.pcbi.1000778
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC2940142/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4895118/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC10398605/
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC9353143/
https://www.mdpi.com/
1422-0067/24/5/4476
https://www.tandfonline.com/doi/
abs/10.1080/10408398.2020.1850417
https://pubmed.ncbi.nlm.
nih.gov/17569223/
https://pubmed.ncbi.nlm.
nih.gov/27012592/
https://www.sciencedirect.com/topics/
biochemistry-genetics-and-molecular-
biology/caspase-3
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC8876821/
https://onlinelibrary.wiley.com/
doi/10.1155/2021/5285841
The recommended number of visual fields to be examined is 150 for a smear size of 3 cm x 2 cm and 100 for a smear size of 2 cm x 1 cm (Note: 150 and 100 visual fields can be designated as '1 length' meaning the visual fields are examined from one end to another)...
The results of acid-fast microscopy may be reported according to the following standards based on the World Health Organization and International Union Against Tuberculosis and Lung Diseases (WHO-IUTLD):
For the Ziehl-Neelsen Method (via light/brightfield microscopy)
No Acid-fast bacilli (AFB) seen - Report as "0". It means no AFB was observed in 2 lengths (i.e., 300 visual fields), thus, conferring a "negative" result.
1-9 AFB in 1 length - Record the actual number of AFB seen (e.g. +1, +2, +9). Note that the plus sign should precede the number. This is also referred to as a scanty positive result.
10-99 AFB in 1 length - Report as "1+". Note that the plus sign should come after the number. This is a positive result.
1-10 AFB per field in at least 50 visual fields - Report as "2+". Note that the plus sign should come after the number. This is a positive result.
More than 10 AFB per field in at least 20 visual fields - Report as "3+". Note that the plus sign should come after the number. This is a positive result and is highly infectious."
https://www.ncbi.nlm.nih.gov/
books/NBK537121/
https://www.sciencedirect.com/science/
article/abs/pii/S0006291X03018904
But while orthomolecular medicine may have its points, the effects of vitamin C on tuberculosis are probably overrated.
As there aren't any clinical or epidemiological studies that prove the benefits of vitamin C as a treatment of tuberculosis, vitamin C believers commonly refer to the following 2013 paper in the most renowned scientific journal, Nature, by Catherine Vilchèze et al:
"Mycobacterium tuberculosis is extraordinarily sensitive to killing by a vitamin C-induced Fenton reaction... Here we show that vitamin C, a compound known to drive the Fenton reaction, sterilizes cultures of drug-susceptible and drug-resistant Mycobacterium tuberculosis, the causative agent of tuberculosis... The bactericidal activity of vitamin C against M. tuberculosis is dependent on high ferrous ion levels and reactive oxygen species production, and causes a pleiotropic effect affecting several biological processes."
https://www.nature.com/
articles/ncomms2898

The original location of the video is on Youtube.
Was this a breakthrough in tuberculosis? Unfortunately not. It's a long, long way from lab dish studies to treating a human disease.
Remember the hype that bleach could kill Covid? It sure does, as a surface disinfectant. And tuberculosis can be killed in lab dishes with vinegar, or alcohol (or bleach, for that matter) much faster than with vitamin C.
The problem is that to get the killing molecules to where the bacteria are, for example the macrophages in the lungs, without greatly damaging the host organism, or even killing it (which surely eradicates the pathogen).

Quote from the paper "Vitamin C Potentiates the Killing of Mycobacterium tuberculosis by the First-Line Tuberculosis Drugs Isoniazid and Rifampin in Mice", for which she is the lead author:
"We previously discovered that high concentrations of vitamin C sterilize cultures of drug-susceptible and drug-resistant Mycobacterium tuberculosis... In vivo, we showed that the vitamin C level in mouse serum can be increased by intraperitoneal injection of vitamin C to reach vitamin C levels close to the concentrations required for activity in vitro... Since... a [inhibitory] dose of 4 mM vitamin C is difficult to achieve in vivo, we tested a subinhibitory concentration of vitamin C (1 mM) added to a combination of INH [isoniazid] and RIF [rifampin]. While INH and RIF combined sterilized a culture of M. tuberculosis within 3 to 4 weeks, the addition of 1 mM vitamin C to this treatment shortened the sterilization time by 7 days."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC5826150/
What amounts of vitamin C are we talking here? Not a few grams of oral vitamin C that may be swallowed per day by an adult human.
"Intravenous (i.v.) or intraperitoneal (i.p.) injections... Aof vitamin C (1 g/kg of body weight) in mice gave maximum plasma concentrations of 15 mM and 7 mM, respectively, whereas the addition of vitamin C to the drinking water of the mice at a dose of 6g/liter only afforded a plasma concentration of 40 μM after 4 weeks. The administration of 4.5 g/kg of vitamin C by i.p. injection was shown to be detrimental to mice, whereas 3 g/kg was well tolerated."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC5826150/
4.5 grams per kg as intraperitoneal (into the abdominal cavity) were detrimental... For a human of 70 kg, this would be 315 grams of vitamin C injected into the abdomen.
In mice, 3 grams per kg were well tolerated. That would be 210 grams injected into a 70 kg human.
And even that megadose worked only together with two highly toxic drugs.
Lab studies really can be misleading, and be the cause of false hope.
Any patient thinking of treating his or her tuberculosis by oral vitamin C, as advocated by vitamin quacks, can rest assured, that this will not have the desired effect.
Tuberculosis and iron
The Germans have a word for it: "verschlimmbessern".
It's untranslatable as a single word, but it has a clear meaning: making something worse while trying to make it better.
And, unfortunately, there is a long history of medical treatments, of tuberculosis and other diseases, that made people worse instead of better. Quackery!
It is well established that tuberculosis is associated with anemia.
"Many patients with active PTB [pulmonary tuberculosis] have low Hb [hemoglobin], and anemia is the most common comorbidity present in TB. According to some study analysis, anemia is evident in 61.53% of TB patients. The overall prevalence of mild, moderate, and severe anemia is 35.67%, 31.1%, and 11.6%, respectively. Furthermore, the prevalence of anemia of chronic disease (ACD) and iron deficiency anemia (IDA) is 49.82% and 20.17%, respectively. Hb levels are low at the time of diagnosis of TB or during the progression of the infection."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC9447415/
Many people will jump to conclusions: let's take iron supplements to solve the anemia issue, and then the tuberculosis may disappear all by itself.
But that won't happen.
"Like all human pathogens, Mtb [Mycobacterium tuberculosis] requires iron for growth and virulence... Mtb iron uptake is a complex process, requiring biosynthesis and subsequent export of Mtb siderophores [Greek: "iron carriers"), followed by ferric iron scavenging and ferric-siderophore import into Mtb... The battle for iron between the human host and bacteria has evolved into a sophisticated cat and mouse game, where bacteria have developed complex pathways to steal iron from host proteins, and to circumvent this, humans have evolved proteins to neutralize bacterial iron-scavenging pathways."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC6568009/
It is a lesser-known function of the immune system to limit iron availability.
"Given the absolute requirement for iron by virtually all human pathogens, an important facet of the innate immune system is to limit iron availability to invading microbes in a process termed nutritional immunity... Iron limitation as an innate immune defense..."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3676888/
Taking iron supplements to alleviate the anemia often seen in tuberculosis patients, is probably not a wise strategy.
"Increase in host Fe levels promotes Mtb [Mycobacterium tuberculosis] growth and tuberculosis (TB) pathogenesis, while Fe-supplementation to latently infected, asymptomatic individuals is a significant risk factor for disease reactivation."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC6722820/
Taking Iron tablets when I'll with tuberculosis is a typical case of "verschlimmbessern".
And maybe not just iron, but other minerals, too.
"Transition metals such as iron, zinc, manganese, and copper have numerous biological roles as both structural and catalytic cofactors for proteins and therefore these metals are essential for life. The importance of transition metals to cellular physiology is underscored by analyses of protein databases, which suggest that approximately 30% of all proteins interact with a metal cofactor. In keeping with the strict requirement for metals in a variety of cellular processes, transition metals are essential for proper vertebrate immune function. Transition metals are also critical for microbial invaders, as bacterial pathogens must acquire nutrient metal in order to cause disease. The strict requirement for these elements during pathogenesis is due to their involvement in numerous processes ranging from bacterial metabolism to accessory virulence factor function. Vertebrates exploit the bacterial requirement for transition metals by sequestering these elements, a concept termed nutritional immunity."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC2847644/
Tuberculosis and ... what was that?
In medicine, small things can sometimes be a game changer.
When Ignaz Semmelweis insisted that physicians wash their hands, he was ridiculed. He died in a psychiatric asylum. Now he is considered a pioneer of hospital medicine, and the hero of mothers-to-be.
Tu Youyou, a Chinese pharmacologist, received the 2015 Nobel Prize in Physiology or Medicine for discovering the anti-malaria drug artemisinin, extracted from an inconspicuous grass, Artemisia annua. She got the lead on that grass from ancient Chinese medical texts.
What if something similar could happen in the context of tuberculosis? And that a solution has been right under our noses, but was unnoticed ever since.
Worldwide there are 2 billion people who are infected with tuberculosis, but only about 10 million annually fall I'll with the disease (0.5 percent). Is there anything specific, present or absent, in the daily routines of people who progress from tuberculosis infection to tuberculosis disease?
Could this information be useful in the treatment of the disease.
Just spinning fantasies... but what were if something as little as drinking tea were to make a huge difference.
Epidemiological studies could find out. And farfetched as it may seem, there have indeed been scientist, from Singapore, looking at the issue. Sober, not in the search of miracles. But still.
"Experimental studies showed that tea polyphenols may inhibit growth of Mycobacterium tuberculosis. However, no prospective epidemiologic study has investigated tea drinking and the risk of active tuberculosis. We investigated this association in the Singapore Chinese Health Study, a prospective population-based cohort of 63,257 Chinese aged 45–74 years recruited between 1993 and 1998 in Singapore. Information on habitual drinking of tea (including black and green tea) and coffee was collected via structured questionnaires. Incident cases of active tuberculosis were identified via linkage with the nationwide tuberculosis registry up to 31 December 2014. Cox proportional hazard models were used to estimate the relation of tea and coffee consumption with tuberculosis risk. Over a mean 16.8 years of follow-up, we identified 1249 incident cases of active tuberculosis. Drinking either black or green tea was associated with a dose-dependent reduction in tuberculosis risk. Compared to non-drinkers, the hazard ratio (HR) ... was 1.01 in monthly tea drinkers, 0.84 in weekly drinkers, and 0.82 in daily drinkers. Coffee or caffeine intake was not significantly associated with tuberculosis risk.
https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC5490523/
Interesting to know in this context how worldwide per capita tea consumption compares with tuberculosis incidence statistics.
Tea consumption per capita
https://en.m.wikipedia.org/wiki/
List_of_countries_by_tea_
consumption_per_capita
Tuberculosis incidences by country
https://data.worldbank.org/
indicator/SH.TBS.INCD
Epidemiological studies are highly relevant for human behavior. They are reliable and actionable. Based on such studies, we may decide to quit smoking, do more exercise, eat no trans fats, use more olive oil in the preparation of our food... or drink more tea.
Biochemists may find out what processes enable a bacterium to persist. That is important and interesting but it is difficult to deduce regimens from biochemical findings, and if one does, one may frequently be wrong. Several decades ago, the propagation of margarine (at that times high in trans fats) as a healthier alternative to butter was based on biochemical theories, and they were debunked by epidemiological studies.
Keeping this in mind, let's check microbiological and biochemical research into tuberculosis and tea.
Mycobacteria make macrophages and similar immune cells their survival niche. Macrophages first detect and ingest the mycobacteria. Inside the macrophages, the bacteria are encapsulated in phagosomes. If everything goes by the script, phagosomes fuse with lysosomes and the bacteria are degraded (killed) by the lysosomes' chemistry.
But mycobacteria manipulate the phagosomes so that they cannot fuse with lysosomes, and thus the bacteria are not killed.
Scientists have elucidated what goes on. Key, apparently, is a coat protein of the phagosomes. This protein is called TACO (tryptophan-aspartate containing coat protein). It is synthesized in macrophages by transcribing certain genes.
Mycobacteria tuberculosis generates chemical signals that lead macrophages to synthesize more TACO than they would normally. Now, if TACO is overly expressed on phagosomes, it inhibits the fusion of phagosomes with lysosomes, and thus, the bacteria are not killed.
The task, thus, would be to inhibit TACO synthesis in macrophages, and then the fusion of phagosomes with lysosomes could run its course, and eliminate the bacteria.
Well, the main phenol in tea, epigallocatechin-3-gallate (EGCG), apparently can do this.
"Laboratory evidence suggests that epigallocatechin-3-gallate (EGCG) in tea leaves... can inhibit the survival of tubercle bacillus within macrophages by inhibiting the TACO (tryptophan-aspartate containing coat protein) gene transcription within macrophages."
Tuberculosis and garlic
Garlic has been a mainstay in traditional healing for centuries, even millennia, anywhere around the world where it grows.
At the turn of the 19th into the 20th century, some Western physicians tried garlic as a treatment for tuberculosis.
"Around the turn of the century, W. C. Minchin, head of the tuberculosis ward at a Dublin hospital, wrote that garlic had a remarkable cure rate for tuberculosis. It was used as an inhalant, taken internally, and applied as a compress and as an ointment. M. W. McDuffie, at approximately the same time in New York City, compared garlic with 55 other treatments for tuberculosis and concluded that it was the most effective."
Quoted from the following pdf file available online:
https://journals.asm.org/doi/pdf/
10.1128/aac.27.4.485
But while sanatorium therapy, even though really expensive, had a perceived good enough success rate with tuberculosis to really take off from the mid-19th century, garlic, even though readily affordable, never convinced enough physicians and patients so that it would enjoy a similar boom.
Garlic may have numerous health benefits, but there are no clinical or epidemiological studies that would prove its effectiveness in alleviating tuberculosis.
There are, however, studies that have tested garlic's effects on tuberculosis in lab dishes and mice.
"Extracts of garlic rich in allicin and ajoene showed appreciable antimycobacterial activity as compared to standard drugs."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4090836/
"Here, we report that allicin/garlic extract exhibits strong anti-mycobacterial responses in vitro and in vivo against drug-sensitive, MDR and XDR strains of TB. In addition to direct killing, allicin also induced pro-inflammatory cytokines in macrophages. Moreover, allicin/garlic extract treatment in murine models of infection resulted in induction of strong protective Th1 response, leading to drastic reduction in mycobacterial burden. These results indicated that allicin/garlic extract has both antibacterial and immunomodulatory activity."
https://www.sciencedirect.com/science/
article/abs/pii/S037887411831763X
The above quote mentions that "allicin also induced pro-inflammatory cytokines in macrophages."
Pro-inflammatory cytokines, such as TNF alpha (tumor necrosis responsible alpha) have a bad rap because they aggravate autoimmune diseases such as rheumatoid arthritis. This is why the pharmaceutical industry has developed TNF inhibitors... But pro-inflammatory cytokines in macrophages are there for a reason. They regulate the destruction of engulfed bacteria.
And a sorry side effect of TNF inhibitors is that in patients using them, a latent tuberculosis infection may become active tuberculosis disease.
"Tumour necrosis factor (TNF) is a potent inflammatory cytokine that plays an important role in immunity to numerous bacterial infections, including Mycobacterium tuberculosis (Mtb), the causative agent of tuberculosis (TB) in humans. [Some drugs] are anti-TNF agents used to treat a range of inflammatory / autoimmune diseases, such as rheumatoid arthritis. The use of some of these drugs has been linked to reactivation TB."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC2940142/
Unlike other, simpler, bacteria, Mycobacterium tuberculosis hijacks macrophages and makes macrophages its primary home. "Tuberculosis and the art of macrophage manipulation"
https://academic.oup.com/femspd/
article/76/4/fty037/4970761?
login=false
And a key tool of Mycobacterium tuberculosis in making macrophages their survival niche is the down-regulation of pro-inflammatory cytokines like TNF (tumor necrosis factor).
"M. tuberculosis can evade antituberculosis (anti-TB) immunity by inhibiting host cell TNF production via expression of specific mycobacterial components."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC4895118/
Thus, if indeed garlic can interfere with Mycobacterium tuberculosis' inhibition of TNF, there may be a role for the plant in a multifaceted anti-tuberculosis regimen, but garlic by itself is probably not a magic tuberculosis cure.
Tuberculosis and durian fruit
Garlic and turmeric have been extensively studied as an intervention against tuberculosis. Durian not.
Durian made its entry into this article via anecdotal evidence.
It was observed that a generous serving of the fruit induced coughing episodes, soon after eating, in a patient with low-key active tuberculosis. There would be enhanced coughing for 10 or 15 minutes, and the lungs would then be clear of phlegm for several hours. The durian ingestion thus acted as an expectorant.
But there is more to durian than just clearing the lungs of mucus. It just happens that out of all foods consumed by humans, durian is by far richest in y-glutamylcysteine (y-EC). y-EC is a precursor to glutathione, a critical molecule in cellular immune function. Glutathione itself is not easily absorbed into cells, but the precursor y-EC is.
"Screening of various plant samples, including fruits, vegetables, and mushrooms, revealed that... for y-EC,
durian pulp displayed the highest level (~6.98 mg/g DW)[DW - dry weight], followed by papaya and tomato (~0.14–0.12 mg/g DW)"
https://www.sciencedirect.com/science/
article/abs/pii/S0889157524000097
"Our findings indicated that y-glutamylcysteine was the preferred form of sulfur storage in durian pulps..."
https://www.sciencedirect.com/science/
article/abs/pii/S0925521423002946
Y-glutamylcysteine (converted intracellularly into glutathione) is a molecule with potential in the treatment of tuberculosis.
"Glutathione Modulates Efficacious Changes in the Immune Response against Tuberculosis... Due to these immunomodulatory properties,
GSH [glutathione] has been hypothesized to be part of an effective adjunctive therapy for
Mycobacterium tuberculosis (M. tb) infection."
https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC10216386/
